
OVARIAN CANCER
Ovarian cancer accounts for about 3% of cancers among women, but it causes more deaths than any other cancer of the female reproductive system.
What are the risk factors for ovarian cancer?
A risk factor is anything that changes your chance of getting a disease like cancer
- Age: The risk of developing ovarian cancer gets higher with age. Ovarian cancer is rare in women younger than 40.
- Obesity: it seems that obese women (those with a body mass index of at least 30) have a higher risk of developing ovarian cancer.
- Reproductive history: Women who have their first full-term pregnancy after age 35 or who never carried a pregnancy to term have a higher risk of ovarian cancer.
- Birth control: Women who have used oral contraceptives (also known as birth control pills or the pill) have a lower risk of ovarian cancer
- Family history of ovarian cancer, breast cancer, or colorectal cancer
Our Videos
Can ovarian cancer be found early ?
Screening tests for ovarian cancer
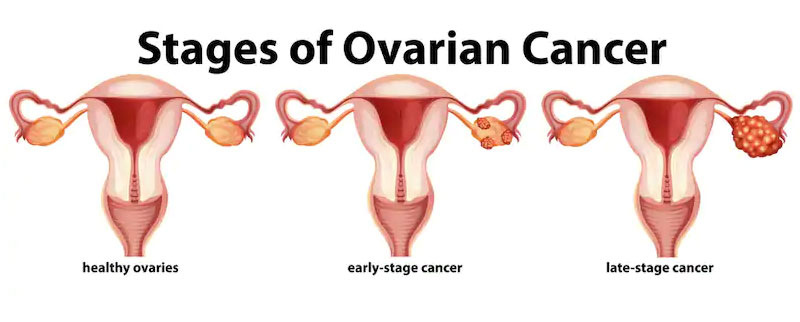
Screening tests and exams are used to detect a disease, like cancer, in people who don’t have any symptoms. There is no effective screening test for ovarian cancer. Early stage Ovarian Cancer can be diagnosed by :
- Transvaginal ultrasound (TVUS)
- CA-125 blood test.
Signs and symptoms of ovarian cancer
The most common symptoms include:
- Bloating
- Pelvic or abdominal pain
- Trouble eating or feeling full quickly
- Urinary symptoms such as urgency (always feeling like you have to go) or frequency (having to go often)
These symptoms are also commonly caused by benign (non-cancerous) diseases and by cancers of other organs. When they are caused by ovarian cancer, they tend to be persistent and represent a change from normal − for example, they occur more often or are more severe. If a woman has these symptoms more than 12 times a month, she should see her doctor, preferably a gynecologist.
Others symptoms of ovarian cancer can include:
- Fatigue
- Upset stomach
- Back pain
- Pain during sex
- Constipation
- Menstrual changes
- Abdominal swelling with weight loss
However, these symptoms are more likely to be caused by other conditions, and most of them occur just about as often in women who don’t have ovarian cancer.
How is ovarian cancer treated?
The main treatments for ovarian cancer are:
- Surgery
- Chemotherapy
- Hormone therapy
- Targeted therapy
- Radiation therapy
Often, 2 or more different types of treatments are used. The choice of treatment depends largely on the type of cancer and the stage of the disease.
Other factors that could play a part in choosing the best treatment plan might include your general state of health, whether you plan to have children, and other personal considerations.
HIPEC (Heated Intraperitoneal Chemotherapy) is a new treatment option for surface epithelial ovarian cancer along with surgery. This gives increased disease free survival. It is available with Max and we are leaders in HIPEC treatment.
What will happen after treatment for ovarian cancer?
Follow-up care
When treatment ends, your doctors will still want to watch you closely. It is very important to go to all of your follow-up appointments.After your cancer treatment is finished, you will probably need to still see your cancer doctor for many years. So, ask what kind of follow-up schedule you can expect.
Key Points
|
Cancer Type
Uterine cancer is the growth of abnormal cells in the lining of the uterus. The lining is called the endometrium.
Uterine cancer usually occurs in women older than 50. The good news is that it is usually cured when it is found early. And most of the time, the cancer is found in its earliest stage, before it has spread outside the uterus.
2. What causes Uterine cancer?
All the causes of Uterine cancer are not known. Doctors believe that hormones that are out of balance often cause the type of Uterine cancer called endometrial carcinoma. The ovaries make most of the female hormones estrogen and progesterone. If the uterus is exposed to too much estrogen over a long period of time, cancer cells may develop.
3. What are the symptoms of Uterine cancer?
These are the most common symptoms of Uterine cancer:
- Unusual bleeding, spotting, or discharge from the vagina
- Any bleeding from the vagina after menopause
- A mass or tumor in the lower abdomen (belly) that can be felt
- Pain in the pelvic area or lower abdomen (belly)
- Unexplained weight loss
These symptoms may be caused by Uterine cancer or several other less serious health problems. If you notice any of them, talk with your doctor right away.
4. What are the risk factors for Uterine cancer?
Certain factors can make you more likely to get Uterine cancer. These are called risk factors. But just because you have one or more risk factors does not mean you will definitely get Uterine cancer. In fact, you can have all the risk factors and still not develop the disease. Or you can have no risk factors and still get Uterine cancer. Here are the main risk factors for Uterine cancer. Many of these risk factors are for endometrial carcinoma. These risks involve having too much exposure to the hormone estrogen:
- Polycystic ovarian syndrome (PCOS). Women with PCOS have abnormal hormone levels. These imbalances can increase the risk of uterine (endometrial) cancer.
- Obesity. Women who are obese get uterine (endometrial) cancer 3 times more often than women who are not obese. Obesity is a leading risk factor for Endometrial cancer. Health conditions linked to obesity, such as diabetes, also increase your risk.
- Early menstruation. Women who had their first period before they were 12 have a higher risk for uterine (endometrial) cancer.
- Late menopause. Women who reach menopause after age 50 have a higher risk for uterine (endometrial) cancer.
- Older age. Most women who get uterine (endometrial) cancer are older than age 50.
- Endometrial hyperplasia. Women who have endometrial hyperplasia have a higher risk of getting uterine (endometrial) cancer. Endometrial hyperplasia means that there are more cells than there should be in the lining of the uterus. This is called a precancerous condition because it might turn into cancer. Women with endometrial hyperplasia may have unusual bleeding.
- No pregnancies. Women who have never been pregnant have a higher chance of uterine (endometrial) cancer.
- Family history of uterine (endometrial) cancer. Women with family members who have had uterine or colon cancer are more likely to get it.
- Previous radiation therapy to the pelvis. If you have had pelvic radiation in the past, your risk for developing Uterine cancer (sarcoma and endometrial) is increased.
- Tamoxifen use. Tamoxifen is a drug used to treat women who have breast cancer and is used to help prevent breast cancer in women at high risk. Women who take tamoxifen have a higher risk of getting uterine (endometrial) cancer.
5. What screening tests are available for Uterine cancer?
There is no standard screening test to find Uterine cancer. A Pap smear, a test routinely used to find cervical cancer, is not very useful in finding Uterine cancer. If you're at high risk for endometrial carcinoma, talk with your doctor about screening tests that might be used.
6. How is a diagnosis of Uterine cancer made?
To check your symptoms, your doctor will ask about your medical history and do a physical examination. This will include a pelvic examination.
An endometrial biopsy is needed to confirm a diagnosis of Endometrial cancer. A biopsy removes a small sample of the lining of the uterus (endometrium) to be looked at under a microscope.
Other tests may include:
- A transvaginal pelvic ultrasound. This uses sound waves to create images of the uterus. The images can show how thick the endometrium is. A thick endometrium can be a sign of cancer in post-menopausal women. Ultrasound also can help show whether cancer has grown into the uterine muscle.
- A hysteroscopy. This allows your doctor to view the inside of the uterus and get an endometrial tissue sample.
- Dilation and curettage (D&C). This test is done to get a sample of tissue from the inside of the uterus. It may be done at the same time as a hysteroscopy.
Testing for Endometrial cancer may show that you haveendometrial hyperplasia. This is not cancer but may develop into cancer.
Tests t
7. If I have Uterine cancer, will I need a hysterectomy?
Surgery to take out the uterus, called a hysterectomy, is the main way to treat most types of Uterine cancer. Sometimes, a hysterectomy can get rid of all the cancer in your body. This is especially true for early stages of endometrial carcinoma. While removing your uterus, your surgeon will usually take out your fallopian tubes and ovaries to stop the production of estrogen. This helps slow or stop the spread of Uterine cancer. Typically, lymph nodes are also removed, to check for the possibility that the cancer has spread. You may have other treatments before or after surgery. These include radiation, hormone therapy, or chemotherapy.
8. What are the treatments for Uterine cancer?
Treatments for Uterine cancer include surgery, radiation therapy, hormone therapy, and chemotherapy.
Surgery is the most common treatment for women with Uterine cancer, and often the only treatment needed. A standard surgery for Endometrial cancer is the removal of the uterus (hysterectomy), with removal of the attached ovaries and fallopian tubes. In many cases, your doctor will also recommend removal of lymph nodes from the abdomen and pelvis to see if the cancer has spread. The complete surgery of hysterectomy with lymph node removal is called surgical staging. Surgical staging can be performed through an incision on your abdomen (laparotomy, open procedure) or by laparoscopy (minimally invasive surgery using cameras to help with the surgery) Your doctor will discuss which approach is best and why.
Radiation uses high-energy beams directed to an area in the body (for Endometrial cancer, the pelvis) to kill cancer cells. Radiation is most frequently used after surgery, but in some cases is used before surgery.
Chemotherapy is the use of anticancer drugs typically administered by vein to kill cancer cells. Chemotherapy is a systemic therapy (travels from head to toe) which works throughout the body, while radiation therapy only works on the area where the radiation is given. Chemotherapy may given to patients whose cancer has spread at the time of their diagnosis or to treat a cancer which comes back (recurs).
Hormone therapy is a type of drug therapy frequently using a class of hormones called progestins. The drugs are given by mouth or by injection. They travel through the body in the blood and can work on special targets on cancer cells called hormone receptors. Hormone therapy is used to treat widespread disease or cancers that return (recur).
9. What are the side effects of surgery ?
If you haven't gone through menopause yet, you'll stop having menstrual periods after surgery, and you won't be able to become pregnant. Also, you may have hot flashes, vaginal dryness, and night sweats. These symptoms are caused by the sudden loss of female hormones. Talk with your doctor or nurse about your symptoms so that you can develop a treatment plan together. There are drugs and lifestyle changes that can help, and most symptoms go away or lessen with time. Surgery to remove lymph nodes may cause lymphedema (swelling) in one or both legs. Your health care team can tell you how to prevent or relieve lymphedema. For some women, a hysterectomy can affect sexual intimacy. You may have feelings of loss that make intimacy difficult. Sharing these feelings with your partner may be helpful.
OVARIAN CANCER
Ovarian cancer accounts for about 3% of cancers among women, but it causes more deaths than any other cancer of the female reproductive system.
What are the risk factors for Ovarian cancer ?
A risk factor is anything that changes your chance of getting a disease like cancer
- Age: The risk of developing ovarian cancer gets higher with age. Ovarian cancer is rare in women younger than 40.
- Obesity: it seems that obese women (those with a body mass index of at least 30) have a higher risk of developing ovarian cancer.
- Reproductive history: Women who have their first full-term pregnancy after age 35 or who never carried a pregnancy to term have a higher risk of Ovarian cancer .
- Birth control: Women who have used oral contraceptives (also known as birth control pills or the pill) have a lower risk of Ovarian cancer
- Family history of Ovarian cancer ,breast cancer or colorectal cancer
Can Ovarian cancer be found early ?
Screening tests for Ovarian cancer
Screening tests and exams are used to detect a disease, like cancer, in people who don’t have any symptoms. There is no effective screening test for Ovarian cancer . Early stage Ovarian cancer can be diagnosed by :
- Transvaginal ultrasound (TVUS)
- CA-125 blood test.
Signs and symptoms of ovarian cancer
The most common symptoms include:
- Bloating
- Pelvic or abdominal pain
- Trouble eating or feeling full quickly
- Urinary symptoms such as urgency (always feeling like you have to go) or frequency (having to go often)
These symptoms are also commonly caused by benign (non-cancerous) diseases and by cancers of other organs. When they are caused by ovarian cancer, they tend to be persistent and represent a change from normal − for example, they occur more often or are more severe. If a woman has these symptoms more than 12 times a month, she should see her doctor, preferably a gynecologist.
Others symptoms of ovarian cancer can include:
- Fatigue
- Upset stomach
- Back pain
- Pain during sex
- Constipation
- Menstrual changes
- Abdominal swelling with weight loss
However, these symptoms are more likely to be caused by other conditions, and most of them occur just about as often in women who don’t have ovarian cancer.
How is ovarian cancer treated?
The main treatments for Ovarian cancer are:
- Surgery
- Chemotherapy
- Hormone therapy
- Targeted therapy
- Radiation therapy
Often, 2 or more different types of treatments are used. The choice of treatment depends largely on the type of cancer and the stage of the disease.
Other factors that could play a part in choosing the best treatment plan might include your general state of health, whether you plan to have children, and other personal considerations.
HIPEC (Heated Intraperitoneal Chemotherapy) is a new treatment option for surface epithelial ovarian cancer along with surgery. This gives increased disease free survival. It is available with Max and we are leaders in HIPEC treatment.
What will happen after treatment for ovarian cancer?
Follow-up care
When treatment ends, your doctors will still want to watch you closely. It is very important to go to all of your follow-up appointments.After your cancer treatment is finished, you will probably need to still see your cancer doctor for many years. So, ask what kind of follow-up schedule you can expect.
Key Points
|
Endometrial cancer
Top 5 risk factors and What Surgery?
It’s becoming increasingly common to hear a near or dear one just diagnosed of Endometrial cancer. For this reason it's important to know why we are seeing more and more cases of Endometrial cancers in India. Dr. Archit pandit a Gynaec oncologist in Delhi , Shalimar Bagh and South Delhi givers us some inputs to understand why Uterine cancers aka Endometrial cancer is so frequently heard of these days .
Lets see what Dr. Archit Pandit one of the best Gynaec oncologists had to say when asked about
Who is at risk of developing Uterine cancer ?
There are mainly who kinds of Endometrial cancer and both have different reasons and risk factors.
Type 1 Endometrial cancer - Type 1 EC’s comprise of around 80% of EC’s and they have better prognosis and outcomes as compared to Type 2 EC’s. Type 1 EC’s are associated with HIGH ESTROGEN LEVELS IN WOMEN. High estrogen levels are seen in the following conditions.
1. ESTROGEN THERAPY without progesterone such as those patients who take Tablets like Tamoxifen (SERM used in Breast cancer patients )
2. ANOVULATORY MENSTRUAL CYCLES - Such as PCOD (polycystic ovarian diseases) , nulliparity (women who have never been pregnant) and infertility. The association in these women is seen mainly because of high frequency of anovulatory cycles in which these women have continuous exposure of estrogen and no opposition of progesterone resulting in higher chances of developing Endometrial cancer .
3. OBESITY - The most important reason to hear about Uterine cancers these days is OBESITY. Inactivity is prevailing much more today as compared to earlier. Obesity is on the rise in India among not only men but women also. Obese women have high levels of Estrogen which in turn can cause EC’s.
4. EARLY MENARCHE & LATE MENOPAUSE — Those women who had early menstruation and also late menopause where exposed to estrogen for a longer time in their menstrual life.
5. HEREDITARY FACTORS - Certain hereditary cancer syndromes such as LYNCH syndrome have 60% lifetime risk of developing EC. If you have a history of Colon-rectal cancers , breast cancer , ovarian cancers , Gastro intestinal cancer history ion you family then one should consult an oncologist who can assess the chances of developing EC.
I’ve been advised Surgery! What surgery should I opt for?
Surgery is usually the main stay of treatment especially in early stage disease. The only way to attempt cure is to perform a surgery. So, if you have been advised surgery it means you have a chance of Cure. Surgery for Endometrial cancer means removing the uterus, both ovaries , cervix and adjacent lymph nodes of the pelvis and para-aortic. Traditionally this surgery was performed by a midline long incision all along the abdomen also called as open surgery. Thanks to changing trends and technology this surgery is now performed by highly skilled surgeons trained in Laparoscopic and Robotic surgery. This is a relatively scarless/minimum scar surgery through which the surgery is performed. The benefits of minimally access surgery are immense such as,
1. Lesser blood loss
2. Early recovery
3. Less pain
4. Relatively scarless
5. Early mobilization and back to work in no time.
6. Lesser chances of lung infections or blood transfusions
7. Better cosmoses as the scars are as small as 4 mm .
Lots of research has supported this approach of performing Radical hysterectomy and pelvic and para aortic lymphadenectomy. This requires specialized training and high quality skill. Dr. Archit pandit is a Gynaec oncologist specifically trained in Laparoscopic and robotic cancer surgeries and has presently performed more than 150 Endometrial cancer surgeries by laparoscopic and robotic technology. Let's see what his patients have to tell about Laparoscopic radical hysterectomy / minimally access surgery for Endometrial cancers and its benefits .




